The Efficacy of Low Dose Nefopam Combined with Fentanyl Injection for Controlling Immediate Postoperative Pain After Laparoscopic Surgery. A Double-blinded, Randomized Controlled Trial
DOI:
https://doi.org/10.69650/ahstr.2024.1229Keywords:
Laparoscopy, Nefopam, Acute Pain ManagementAbstract
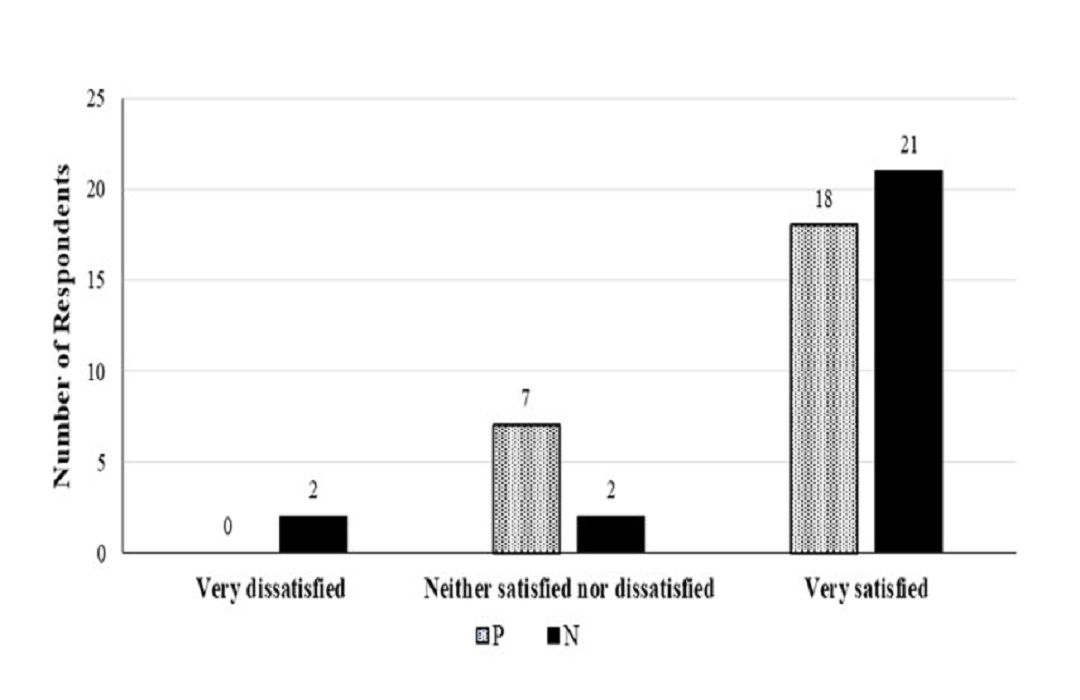
Backgroud: Despite the widespread use of laparoscopic surgery across various procedures, effective postoperative pain management remains a challenge. Nefopam may be effective as an adjuvant analgesic for acute postoperative pain control. Objective: This study highlights the analgesic effects and risk of adverse events when using a low dose nefopam for laparoscopic surgical procedures. Methods: This study is double-blinded, prospective randomized controlled trial. There were 50 subjects who were divided into 2 groups. The nefopam group (n=25) received slow intravenous (IV) injection of 10 mg nefopam and IV 25 mcg fentanyl immediately in post-anesthetic care unit (PACU), while the placebo group (n=25) received IV isotonic saline and IV 25 mcg fentanyl. The primary outcomes include the numerical rating scales (NRS) of postoperative pain intensity, fentanyl consumption, adverse effects and patient satisfaction in PACU. Results: There was no difference in demographic data between groups. The NRS scores of the nefopam group at 30, 45 and 60 minutes postoperative were significantly lower than of the placebo group (p ˂ 0.05). The amount of fentanyl consumption in PACU is comparable between groups (p = 0.311). Patients in both groups experienced some adverse effects including nausea, vomiting, tachycardia, dry mouth, and dizziness, however the incidence was not different between groups. Additionally, the nefopam group tended to have better patient satisfaction. Conclusion: The additional low dose nefopam administered by slow IV injection could reduce acute pain intensity after laparoscopic abdominal surgery, while this approach did not increase the risk of adverse effects.
References
Apfel, C. C., Heidrich, F. M., Juka-Rao, S., Jalota, L., Hornuss, C., Whelan, R. P., Zhang, K., & Cakmakkaya, O.S. (2012). Evidence-based analysis of risk factors for postoperative nausea and vomiting. British Journal of Anaesthesia, 109(5), 742-753. https://doi.org/10.1093/bja/aes276
Baltes, B. J. (1977). Gastrointestinal blood loss study with a new analgesic compound: nefopam hydrochloride. The Journal of Clinical Pharmacology, 17(2-3), 120-124. https://doi.org/10.1002/j.1552-4604.1977.tb04597.x
Bhatt, A. M., Pleuvry, B. J., & Maddison, S. E. (1981). Respiratory and metabolic effects of oral nefopam in human volunteers. British Journal of Clinical Pharmacology, 11(2), 209-211. https://doi.org/10.1111/j.1365-2125.1981.tb01126.x
Bisgaard, T. (2006). Analgesic treatment after laparoscopic cholecystectomy: a critical assessment of the evidence. Anesthesiology, 104(4), 835-846. https://doi.org/10.1097/00000542-200604000-00030
Djerada, Z., Fournet-Fayard, A., Gonzalo, C., Lelarge, C., Lamiable, D., Millart, H., & Malinovsky, J. M. (2014). Population pharmacokinetics of nefopam in elderly, with or without renal impairment, and its link to treatment response. British Journal of Clinical Pharmacology, 77(6), 1027-1038. https://doi.org/10.1111/bcp.12291
Dordoni, P. L., Della, Ventura, M., Stefanelli, A., Iannace, E., Paparella, P., Rocca, B., & Accorra, F. (1994). Effect of ketorolac, ketoprofen and nefopam on platelet function. Anaesthesia, 49(12), 1046-1049. https://doi.org/10.1111/j.1365-2044.1994.tb04352.x
Du, Manoir, B., Aubrun, F., Langlois, M., Le, Guern, M. E., Alquier, C., Chauvin, M., & Fletcher, D. (2003). Randomized prospective study of the analgesic effect of nefopam after orthopaedic surgery. British Journal of Anaesthesia, 91(6), 836-841. https://doi.org/10.1093/bja/aeg264
Evans, M. S., Lysakowski, C., & Tramèr, M. R. (2008). Nefopam for the prevention of postoperative pain: quantitative systematic review. British Journal of Anaesthesia, 101(5), 610-617. https://doi.org/10.1093/bja/aen267
Girard, P., Chauvin, M., & Verleye, M. (2016). Nefopam analgesia and its role in multimodal analgesia: a review of preclinical and clinical studies. Clinical and Experimental Pharmacology and Physiology, 43(1), 3-12. https://doi.org/10.1111/1440-1681.12506
Guirimand, F., Dupont, X., Bouhassira, D., Brasseur, L., & Chauvin, M. (1999). Nefopam strongly depresses the nociceptive flexion (R(III)) reflex in humans. The Journal of the International Association for the Study of Pain, 80(1-2), 399–404. https://doi.org/10.1016/s0304-3959(98)00238-3
Heel, R. C., Brogden, R. N., Pakes, G. E., Speight, T. M., & Avery, G. S. (1980). Nefopam: a review of its pharmacological properties and therapeutic afficacy. Drugs, 19, 249-267. https://doi.org/10.2165/00003495-198019040-00001
Hwang, B. Y., Kwon, J. Y., Lee, D. W., Kim, E., Kim, T. K., & Kim, H. K. (2015). A randomized clinical trial of nefopam versus ketorolac combined with oxycodone in patient-controlled analgesia after gynecologic surgery. International Journal of Medical Scencesi, 12(8), 644-649. https://doi.org/10.7150/ijms.11828
Jin, H. S., Kim, Y. C., Yoo, Y., Lee, C., Cho, C. W., & Kim, W. J. (2016). Opioid sparing effect and safety of nefopam in patient controlled analgesia after laparotomy: a randomized, double blind study. Journal of International Medical Research, 44(4), 844-854. https://doi.org/10.1177/0300060516650783
Kapfer, B., Alfonsi, P., Guignard, B., Sessler, Daniel, I., & Chauvin, M. (2005). Nefopam and ketamine comparably enhance postoperative analgesia. Anesthesia & Analgesia, 100(1), 169-174. https://doi.org/10.1213/01.ANE.0000138037.19757.ED
Kim, E. M., Jeon, J. H., Chung, M. H., Choi, E. M., Baek, S. H., Jeon, P. H., & Lee, M. H. (2017). The Effect of Nefopam Infusion during Laparoscopic Cholecystectomy on Postoperative Pain. International Journal of Medical Sciences, 14(6), 570-577. https://doi.org/10.7150/ijms.19021
Kim, K., Kim, W. J., Choi, D. K., Lee, Y. K., Choi, I. C., & Sim, J. Y. (2014). The analgesic efficacy and safety of nefopam in patient-controlled analgesia after cardiac surgery: a randomized, double-blind, prospective study. Journal of International Medical Research, 42(3), 684-692. https://doi.org/10.1177/0300060514525351
Lee, J. H., Kim, J. H., & Cheong, Y. K. (2013). The analgesic effect of nefopam with fentanyl at the end of laparoscopic cholecystectomy. The Korean Journal of Pain, 26(4), 361-367. https://doi.org/10.3344/kjp.2013.26.4.361
Luo J, Min S. (2017). Postoperative pain management in the postanesthesia care unit: an update. Journal of Pain Research, 16(10), 2687-2698. https://doi.org/10.2147/JPR.S142889
Martinez, V., Beloeil, H., Marret, E., Fletcher, D., Ravaud, P., & Trinquart, L. (2017). Non-opioid analgesics in adults after major surgery: systemic review with network meta-analysis of randomized trials. British Journal of Anaesthesia, 118(1), 22-31. https://doi.org/10.1093/bja/aew391
Maund, E., McDaid, C., Rice, S., Wright, K., Jenkins, B., & Woolacott, N. (2011). Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs for the reduction in morphin-related side-effects after major surgery: a systematic review. British Journal of Anaesthesia, 106(3), 292-297. https://doi.org/10.1093/bja/aeq406
Mimoz, O., Incagnoli, P., Josse, C., Gillon, M. C., Kuhlman, L., Mirand, A., Soilleux, H., & Fletcher, D. (2001). Analgesic efficacy and safety of nefopam vs propacetamol following hepatic resection. Anaesthesia, 56(6), 520-525. https://doi.org/10.1046/j.1365-2044.2001.01980.x
Moon, J. Y., Choi, S. S., Lee, S. Y., Lee, M. K., Kim, J. E., Lee, J. E., & Lee, S. H. (2016). The effect of nefopam on postoperative fentanyl consumption: a randomized, double-blind study. The Korean Journal of Pain, 29(2), 110-118. https://doi.org/10.3344/kjp.2016.29.2.110
Na, H. S., Oh, A. Y., Koo, B. W., Lim, D. J., Ryu, J. H., & Han, J. W. (2016). Preventive analgesic efficacy of nefopam in acute and chronic pain after breast cancer surgery: a prospective, double-blind, and randomized trial. Medicine, 95(20), 1-6. https://doi.org/10.1097/MD.0000000000003705
Novelli, A., Díaz-Trelles, R., Groppetti, A., & Fernández-Sánchez, M. T. (2005). Nefopam inhibits calcium influx, cGMP formation, and NMDA receptor-dependent neurotoxicity following activation of voltage sensitive calcium channels. Amino Acids, 28, 183-191. https://doi.org/10.1007/s00726-005-0166-0
Park, S. K., Yoo, S., Kim, W. H., Lim, Y. J., Bahk, J. H., & Kim, J. T. (2018). Association of nefopam use with postoperative nausea and vomiting in gynecological patients receiving prophylactic ramosetron: a retrospective study. PLOS One, 13(7). https://doi.org/10.1371/journal.pone.0201084
Remérand, F., Le, Tendre, C., Rosset, P., Peru, R., Favard, L., Pourrat, X., Laffon, M., & Fusciardi, J. (2013). Nefopam after total hip arthroplasty: role in multimodal analgesia. Orthopaedics & Traumatology: Surgery & Research, 99(2), 169-174. https://doi.org/10.1016/j.otsr.2012.08.007
Son, J. S., Doo, A., Kwon, Y. J., Han, Y. J., & Ko, S. (2017). A comparison between ketorolac and nefopam as adjuvant analgesics for postoperative patient-controlled analgesia: a randomized, double-blind, prospective study. Korean Journal of Anesthesiology, 70(6), 612-618. https://doi.org/10.4097/kjae.2017.70.6.612
Sunshine, A., & Laska, E. (1975). Nefopam and morphine in man. Clinical Pharmacology & Therapeutics, 18(5), 530-534. https://doi.org/10.1002/cpt1975185part1530
Tramoni, G., Viale, J. P., Cazals, C., & Bhageerutty, K. (2003). Morphine-sparing effect of nefopam by continuous intravenous injection after abdominal surgery by laparotomy. European Journal of Anaesthesiology, 20(12), 984-992. https://doi.org/10.1017/s0265021503251590
Yoon, J. U., Byeon, G. J., Cheon, J. H., Choi, Y. M., Ri, H. S., & Baik, S. W. (2016). Post-operative intravenous patient-controlled analgesic efficacy of morphine with ketorolac versus nefopam after laparoscopic gynecologic surgery; a randomized non-inferiority trial. Korean Journal of Anesthesiology, 69(2), 161-166. https://doi.org/10.4097/kjae.2016.69.2.161
Zhao, T., Shen, Z., & Sheng, S. (2018). The efficacy and safety of nefopam for pain relief during laparoscopic cholecystectomy: a meta-analysis. Medicine, 97(10), 1-10. https://doi.org/10.1097/MD.0000000000010089
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Asian Health, Science and Technology Reports

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.